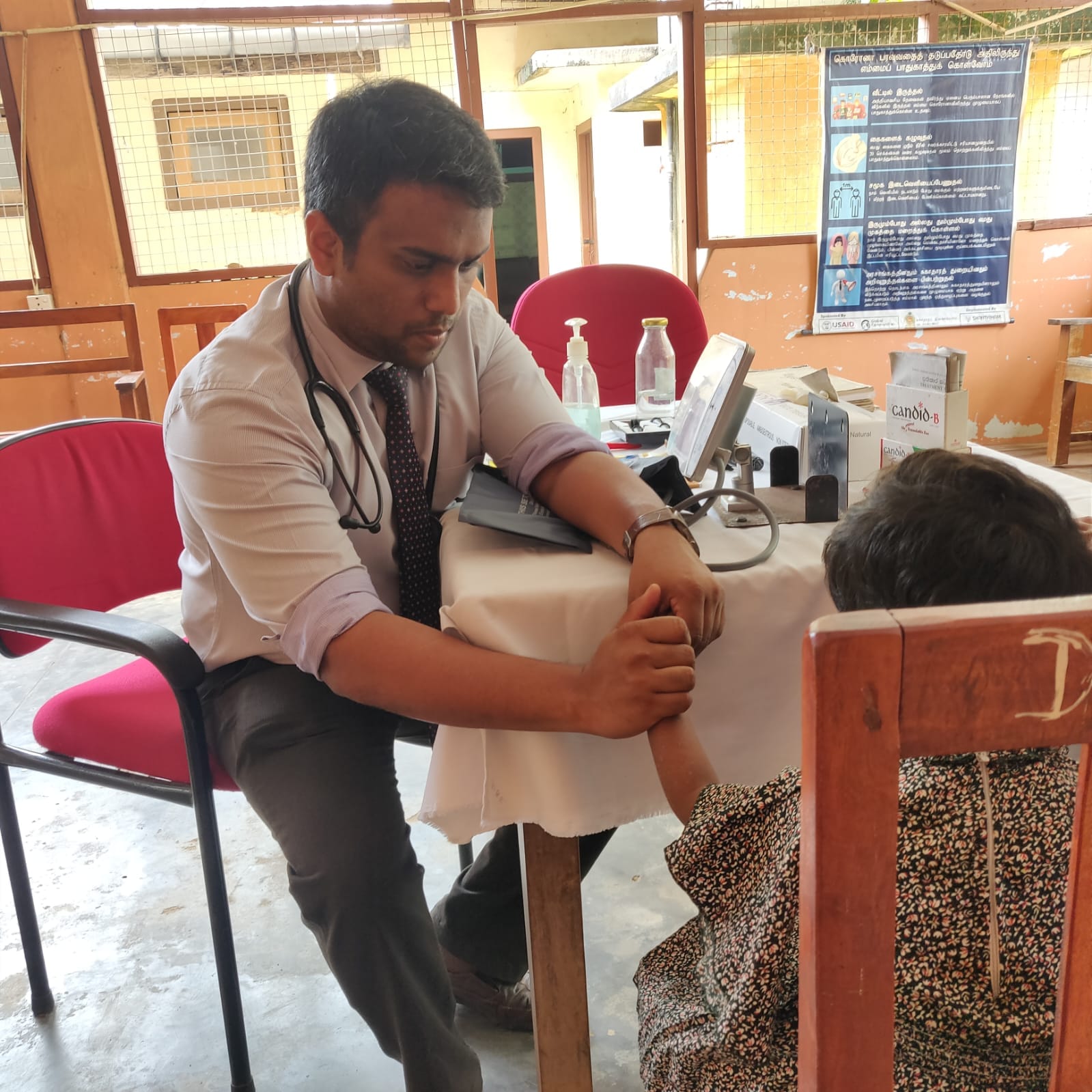
At Kilinochchi District General Hospital, something significant was happening without much fanfare. Dr. Sivalingarajah Raguraman—a consultant obstetrician who teaches at the University of Jaffna and graduated from there himself—was at the center of it all. He's the kind of person who doesn't need to announce his presence in a room, but you notice him anyway. Tall, thoughtful, with the quiet confidence of someone who knows his purpose.
They were opening a subfertility clinic and IVF center—the first one Kilinochchi has ever had. It might not sound like much to outsiders, but for couples who have been struggling to have children, this place represents something they've been searching for: a real chance.
This isn't just another medical facility opening its doors. For families who have carried the weight of unfulfilled hopes, who have watched friends and siblings welcome babies while they waited, this center means they finally have somewhere to turn.
As I spoke with Dr. Raguraman, the scale of the problem struck me hard. Subfertility—defined as the inability to conceive after 12 months of regular unprotected intercourse—is rising sharply, both globally and in Sri Lanka. “We are seeing a surge in male patients with absolutely zero sperm counts,” he shared. Among them are long-distance drivers exposed to chronic heat conditions that elevate scrotal temperature and damage sperm production. He linked this trend to a more unsettling global phenomenon: climate change. “Sperm counts in men have halved since the 1980s, paralleling the rise in greenhouse gases,” he noted grimly. “The day may come when all reproduction will depend on laboratory techniques.”
As a family physician, I witness echoes of this in my own clinic—couples from both North and South who come seeking help after years of fruitless attempts to conceive. Polycystic ovarian disease (PCOD), often associated with obesity, is a leading culprit among women. Pelvic infections, fibroids, and ovulatory dysfunctions are common. Among men, low sperm counts, poor motility, and erectile dysfunction are becoming alarmingly prevalent.
Sri Lanka is facing a birth drought. The fertility rate has dropped by nearly 30% in the past year alone. While the reasons are complex—ranging from economic hardship, lifestyle choices, and delayed marriages to climate-related impacts.
Nowhere is this crisis more pronounced than in the Northern Province. In Jaffna, a staggering 23.1% of couples are subfertile—nearly one in four. Primary subfertility accounts for 18.8%, while secondary subfertility—couples who have had at least one child but struggle to conceive again—contributes another 4.4%. These figures are the highest in the country.
Even more troubling is the fact that nearly two-thirds of these couples are not receiving any treatment. Of those who once sought help, many have since given up—defeated by financial, social, and systemic barriers.
Subfertility is not just a medical issue; it’s a profound psychosocial burden. In the conservative culture of Northern Sri Lanka, women often bear the brunt of the blame, leading to stigma, depression, and even marital instability. At Teaching Hospital Jaffna, studies show that among subfertile women, 34.1% experience severe depression, 47.5% report anxiety, and 24.4% struggle with stress. Many couples delay treatment for years—on average, over five years—because of low awareness, shame, cost, and poor referral systems. By then, age has eroded their already fragile chances of conceiving.
The economic toll is equally devastating. IVF and other advanced fertility treatments cost upwards of 3 to 4 million Sri Lankan rupees—a price tag well beyond the reach of most. Some couples turn to India for lower-cost care. Others—those without money or support—turn to God, or to less scrupulous "healers." Dr. Raguraman recounts heartbreaking stories of couples exploited by shamans, priests, and even rogue clinics that fail to maintain basic standards. “The medical mafia makes it nearly impossible to do good without expecting something in return,” he laments.
Yet he fights on.
Together with his team, Dr. Raguraman has led a community-driven, context-specific response tailored to the realities of Northern Sri Lanka. Guided by the FIGO Fertility Toolbox, the approach operates on three levels—primary, intermediate, and advanced.
At the primary care level, community health workers (CHWs), trained from Mothers’ Support Groups, conduct fertility awareness campaigns, identify subfertile couples, and connect them with family physicians. In Nallur MOH alone, CHWs held 49 awareness programs reaching nearly 900 individuals. Of 78 identified cases, 18 accessed primary care and 11 progressed to specialist services.
At the intermediate level, a dedicated Women's Health Centre was opened at the Teaching Hospital, Jaffna, in 2024—donated by the Sivapoomi Trust and equipped by the Abayam Foundation. Here, a multidisciplinary team offers basic fertility evaluations and treatments, including ovulation induction and intrauterine insemination (IUI). In three years, 943 couples registered. IVF success rates were 23.9%, while other methods also showed promising outcomes—yet 37% of couples were unable to afford IVF.
At the advanced level, Sri Lanka’s public sector remains starkly under-equipped. Advanced services like IVF are largely monopolized by expensive private clinics. However, a beacon of hope lies in the pipeline: an Assisted Reproductive Technology Simulation Lab (ARTS-lab) at the University of Jaffna and a proposed IVF Centre at the Kilinochchi Women’s Health Centre, designed as a future Centre of Excellence.
Dr. Raguraman’s team isn’t stopping there. With support from international donors, they plan to scale up services across the entire Northern Province. A stepped-wedge cluster randomized trial—considered a gold standard for health service evaluations—will help measure impact as services expand district by district. Satellite CHW-based fertility units, intermediate women’s centres, and an integrated IVF hub are envisioned for the near future.
At the heart of it all lies a simple, universal truth: the desire to have a child is a basic human right. “Every couple deserves a chance to build a family,” Dr. Raguraman says. “This is how we give back to our people—not just through treatment, but by restoring hope.”
Birth rates are dropping worldwide. Climate change is rewiring human biology in ways we're only beginning to understand. Economic uncertainty has young couples postponing the families they've always wanted. In this shifting landscape, the ability to have children has become something precious and precarious.
That's what makes doctors like Raguraman so vital. They understand that every percentage point in those fertility statistics represents real people—couples who lie awake at night wondering if they'll ever hear a child call them mom and dad. Each embryo in those IVF labs carries the weight of someone's deepest hope, the answer to prayers whispered in the dark.
In a world that sometimes feels like it's forgetting how to hope, places like this remind us what we're really fighting for.